Popular Articles
- Listol Supplement Facts
- 9 ADHD Products Reviewed
- 5 Natural Alternatives to Adderall
- Listol Interactions
- Helpful ADHD Vitamins & Attention Vitamins
- Cyntol Supplement Facts
- ADHD Herbs - Guarana and Other Herbal Supplements
- ADHD Product Review - Synaptol
- Supplements to Improve Short Term Memory
- Pills for Memory
- More Articles ...
 Natural Supplements that Enhance MemoryIn This Article
Memory is how we remember old facts and learn new information. When memory is impaired, it can lead to repeated forgetfulness which is the first stage of cognitive decline. Although there are many prescription and over-the-counter memory pills available in pharmacies, a lot of them do not significantly improve memory. Before you go looking for more memory pills, consider natural supplements. They are safe and well-tolerated. This article discusses the most effective natural supplements to look out for if you want to enhance your memory.
Memory loss ranges from regular forgetfulness to full-on dementia. It is quickly becoming a costly public health crisis as the number of people affected increases yearly. While memory loss is often linked with aging, it does affect young people too and it is avoidable even in the elderly. The brain stores information as memories. Most of the processes involved in encoding and storing memories happen while we sleep and these processes require the linkage of new information to old ones. The processes required for memory formation involve an intricate network of neurons and the synapses that link them together. Also, the transfer of information between these nerves goes through a set of chemical messengers known as neurotransmitters. Concerning memory, the most important neurotransmitter is acetylcholine. Also, the most important memory seats are the amygdala, hippocampus, and different sites in the medial temporal lobe. Memory loss is caused by damage to the neurons and neurotransmitter pathways involved in encoding, storing, and retrieving memories. Additionally, any factor that reduces the amount or activity of acetylcholine will interfere negatively with memory. Therefore, the drugs and supplements used to enhance memory work by preventing damage to the memory seats of the brain and also by improving the acetylcholine pathways in the brain. While conventional prescription drugs may temporarily enhance memory, they come with several side effects and their benefits are only short-lived. In contrast, natural supplements do not work instantly; in fact, these supplements are only beneficial with long-term therapy. However, they are safer, effective, and well-tolerated. In recent years, more attention has turned to natural supplements as memory boosters. In this regard, there have been multiple clinical studies to assess the efficacies and safeties of these supplements. Such clinical investigations are important given the number of over-the-counter memory pills that are formulated from natural supplements. This article discusses the most effective natural supplements that can enhance memory. VitaminsB VitaminsThe B vitamins are essential to many biochemical and physiological processes in the body. They are needed for every cellular event from metabolism and enzymatic reactions to DNA regulation and immune system modulation.
Even more important is the effect these vitamins have on the homocysteine level in the body. Homocysteine is a metabolic intermediate in amino acid synthesis. When some of the B vitamins are lacking the synthesis gets stuck at homocysteine. However, homocysteine is a toxic intermediate and it has been shown to damage neurons (and the heart). Therefore, B vitamins serve a protective role in the central nervous system by keeping homocysteine levels low in brain cells. Of the B vitamins, vitamins B6, B9, and B12 are the most important for memory. Vitamin B9 and B12 deficiencies are strongly associated with cognitive decline and memory loss. In a large-scale study published in the American Journal of Clinical Nutrition, each of the 700 volunteers recruited was given either a placebo or a combination of vitamins B9 and B12. The study result showed that the vitamin combination was effective for improving short-term memory after 24 months. Both vitamins work by driving the conversion of homocysteine to methionine and preventing the accumulation of the neurotoxic (and cardiotoxic) intermediate. The Antioxidant VitaminsThe antioxidant vitamins include vitamins A (the beta-carotene form), C, and E.
These vitamins reduce oxidative stress in the central nervous system by mopping up the harmful free radicals and reactive oxygen species that may damage nerves and other brain structures. Because they protect these nerves, the antioxidant vitamins preserve the chain of communication and the extensive neural networks that are necessary for the encoding, storage, and retrieval of memories. Besides this antioxidant property, each of these vitamins also improves cognitive functions in other ways. For example, vitamin E improves blood circulation in the brain and, therefore, can enhance memory by increasing the supply of oxygen and nutrients to the centers of memory in the brain. Vitamin DVitamin D is fast becoming the darling vitamin of the decade. New frontiers of research into the uses of the vitamin are revealing wholly new benefits. For example, vitamin D has been proven to possess anti-inflammatory, antimicrobial, and even immunomodulatory properties. Likewise, researchers are getting a clearer understanding of their close ties to memory. First, vitamin D deficiency causes short-term memory loss. Secondly, the discovery that vitamin D receptors are concentrated in the parts of the brain controlling memory is another good indication that the vitamin is important to memory. True to this theory, some studies have established that taking vitamin D supplements can improve concentration, working memory, and mental capacity. MineralsMagnesiumThe most important link between magnesium and ADHD is that some of the symptoms of magnesium deficiency especially in children are also ADHD symptoms. These shared symptoms include irritability, mental confusion, shortened attention span, and inability to focus on tasks for long periods. This is the basis of all studies examining magnesium levels in ADHD children. Supplementation with magnesium was found to improve ADHD symptoms in some children. The recommended dose of magnesium supplements in ADHD treatment is 200 mg per day. However, it is important to talk to your doctor before starting on magnesium supplements since magnesium can disrupt the absorption and effect of certain antibiotics and antihypertensive drugs. How It WorksMagnesium calms the central nervous system, which is important in children with hyperactivity symptoms. The body utilizes magnesium to help transmit messages throughout the nervous system. Magnesium is a key factor in the production of serotonin, which is an important neurotransmitter that promotes wellbeing. Low levels of serotonin are usually associated with moodiness, irritability, and depression. With adequate amounts of magnesium in the body, children can think without any difficulty and focus better. It also promotes concentration and improves attentiveness. Children with attention disorder usually have lower magnesium levels. Taking magnesium supplements can effectively help in alleviating hyperactive behavior and improve focus and attention. People with ADHD have differences in their metabolism, and they need natural ADHD supplements to help control this magnesium shortage. Magnesium also relaxes the body. It is required for the relaxation of nerves and muscles. In the absence of adequate minerals in the body, spasms and twitches are common problems. A calm body promotes emotional well-being and soothes the mind. It reduces the feeling of uneasiness that causes hyperactive children to become agitated. Other Health Benefits of MagnesiumMagnesium aids in regulating blood sugar levels. It aids in absorbing and utilizing other vital minerals and nutrients. It is known to activate enzymes that handle nutrient absorption, hormone production, energy production, and much more. It is also a potent antioxidant that protects from free radical damage. All these aspects of magnesium can improve the overall health of your children and effectively alleviate ADHD symptoms. Natural Sources of MagnesiumThe best way to ensure that your child gets an adequate amount of magnesium is to give magnesium-rich foods. Although a magnesium-rich diet is suggested, most parents of ADHD inflicted children find it helpful to include magnesium supplements. The best way to ensure that your child gets an adequate amount of magnesium is to use magnesium citrate powder that can be mixed easily in pure fruit juice without affecting the taste too much. You may also consider using natural ADHD treatment options such as Listol, which contains magnesium among other safe and natural ingredients. For more information on ADHD treatments, read these articles: Zinc & ADHD, B Vitamins for ADHD, and Vitamin B12 & ADHD. SeleniumSelenium is an antioxidant mineral. It is famously known for the protein complexes it forms. These complexes make up a family of selenoproteins which serve as antioxidant enzymes and cofactors. Therefore, selenium can help mop up reactive oxygen species and other free radicals from the brain. This protective effect can improve memory considerably. Lastly, the antioxidant effect of selenium improves and is improved by, the antioxidant effect of vitamin E. Therefore, a combination of the two nutrients can greatly enhance memory. CalciumCalcium is an essential mineral that is especially important for signal transmission between cells. In the central nervous system, calcium is required for nerve cells to release neurotransmitters and in the muscle cells, it promotes contraction. Calcium is also an important cofactor for many enzymes especially those involved in blood clotting. Most of the calcium found in the body is stored in the bones where the mineral is required for bone formation. The bone then releases calcium into the blood either as free ions or bound with proteins such as albumin.
The richest dietary sources of calcium are milk and milk products such as cheese, ricotta, and yogurt. Other good sources of the mineral are seaweeds, hazelnut, almond, lentils, figs, wheat germ, eggs, flour, brown sugar, and orange. The recommended daily intake value of calcium varies with age. For children, the recommended daily calcium intake is 1000 mg per day or less. Adults can take 1000 – 1500 mg of calcium per day. When calcium levels go below the normal range, it causes a deficiency condition known as hypocalcemia. Calcium supplements are used to correct hypocalcemia. The expert recommendation is that calcium supplements should be taken with food. Also, no more than 600 mg of calcium should be taken at once. This is because calcium absorption actually reduces as the amount of calcium available for absorption increases. Vitamin D may be added to calcium supplementation to improve the absorption of the mineral. Various salts of calcium are used to make calcium supplements. Even antacids that contain calcium carbonate qualifies as a calcium supplement. Other salts include calcium carbonate, calcium lactate, calcium phosphate, calcium malate, calcium fumarate, and calcium aspartate. How Calcium Affects MemoryCalcium is especially important for signal transduction in cells. For this reason, it is sometimes called a second messenger. Coupled with the fact that calcium is necessary for neurons to release neurotransmitters in the brain, calcium plays an important role in the areas of the brain responsible for storing and retrieving memory. The best way to see what effects calcium has on memory is to study the memory loss that happens when calcium levels fall. Calcium channel blockers make a class of drugs used to lower blood pressure. Although they have been used for a long time with considerable success, over the last few years, there have been increasing reports of long-term side effects of these drugs.
In a surprise finding, a 1997 paper published in the Journal of American Geriatrics Society detailed the kind of damage calcium channel blockers does to the brain. This study was sponsored by the National Heart Lung and Blood Institute. It was initiated in 1989 and it involved almost 6000 elderly patients receiving calcium channel blockers. The brain damage caused by these drugs was first detected by MRI (magnetic resonance imaging) scans and confirmed by memory tests. In the MRI scan, the area of the brain-damaged correlated to the parts of the brain known to be the seat of memory. The damage was described as white matter hyperintensity. The study also showed that both short-acting and long-acting calcium channel blockers caused memory loss. Similar reports of memory loss due to brain damage have been published for other drugs that lower calcium levels in the body. Another important class of drugs known to cause this long-term damage belongs to the class of diuretics called loop diuretics (Lasix belongs to this drug class). Another link between calcium and memory loss involves the plasma proteins (albumin is a prime example) that bind calcium in the body. Free, unbound calcium can be toxic to brain cells, therefore, high levels of calcium ions in the brain can also cause brain loss. In fact, when excess calcium ions enter cells, they kill off those cells. In the brain, the influx of calcium ions into nerve cells triggers the over-excitation of neural circuits. The amplified electrical stimulation destroys neurons. When this occurs in the memory seats of the brain, the resultant brain damage causes progressive memory loss. This mechanism contributes to cognitive decline due to aging. This is because as we grow older, the body produces less of the proteins that bind to calcium, and the number of free calcium ions that get into brain cells increases. Studies on Calcium and Memory LossThe following discussion is only a summary of studies done on the link between calcium and memory loss. In a 2010 study published in the Pflugers Archiv European Journal of Physiology, the author linked calcium with the neurodegeneration that occurs during Alzheimer’s disease and the memory loss that results from it. This report identified the metabolites of beta-amyloid protein precursor as the cause of learning deficits and memory loss. These metabolites act by influencing how calcium ions mediate the signal transduction. One way by which the metabolites act is by increasing the number of calcium ions in brain cells. The result is that the changes made in calcium-mediated signal transduction prevent the storage of new memories. While this study demonstrates that abnormally high levels of calcium ions in brain cells can cause memory loss, the next study underscores the importance of calcium to the retention and retrieval of long-term memory. This 1999 study was published in the journal, Neuron. This study involved mice and studied the importance of calcium-mediated signal transduction in the hippocampus. The hippocampus is known to be one of the parts of the brain responsible for memory and learning. This study identifies the sequence of events needed for the preservation of long-term memory. It begins with calcium stimulating the release of two enzymes in the hippocampus. These enzymes are both adenylyl cyclases and they produce cAMP (cyclic adenosine monophosphate) which then powers the signaling mechanisms needed for forming long-term memories. A 2008 study published in The Journal of Neuroscience builds on the findings of the Neuron study. The researchers identified that calcium-mediated increase in cAMP levels is under the control of a transcription factor called CaMKIV (calcium/calmodulin-dependent protein kinase IV). By increasing the levels of CaMKIV in the hippocampus, the researchers were able to increase learning and enhance the storage of social and contextual memories in the mice used in the study. Since CaMKIV levels decline as we age, it is believed to be a major cause of age-related memory loss. By increasing CaMKIV levels, it is possible to reverse cognitive decline due to aging and enhance the ability to form long-term memory. Calcium Supplementation for Memory LossCalcium supplements can only improve memory loss in people who suffer from hypocalcemia.
Definitely, there are other areas of calcium-dependent pathways to exploit to fully treat memory loss. People who have normal levels of calcium should not take up calcium supplementation to reverse memory loss. This is because abnormally high levels of calcium can be toxic to cells (both in the brain and the rest of the body). For the elderly, it seems that high calcium level rather than low calcium level is a stronger cause of memory loss and dementia symptoms. Therefore, calcium supplementation should be closely monitored in this age group and immediately discontinued at the first sign of cognitive decline. Also, older adults usually have lower levels of calcium-binding plasma proteins. Without these proteins, unbound calcium ions become neurotoxic. The obvious solution is to replace the missing binding proteins with a safe alternative. Such an alternative is provided by a natural supplement supplying related and substitute proteins extracted from jellyfish. IronStudies have proved that nearly 8% of children aged 4 years and below have an iron deficiency. This percentage rises to 13% in children aged between 5 and 12 and then settles back to 8% in individuals above the age of 15. Anemia is the common repercussion of iron deficiency. Even minor iron deficiency may affect the thyroid, weaken the immune system, and mess up with physical performance. It has also been implicated in several neurological and psychiatric conditions, including ADHD (attention deficit hyperactive disorder) and learning disabilities. The link between iron deficiency and ADHD should be considered if you have a child with ADHD symptoms. You can support ADHD treatment by giving iron supplements to your child. Lack of certain minerals such as zinc, magnesium, and iron can stimulate impulsiveness, carelessness, and hyperactivity in kids. Thus, an adequate amount of iron consumption is essential to improve neurological conditions, including ADHD and other learning disorders. Iron and the Human BodyIron is an essential mineral in humans because it is needed for the proper formation and functioning of red blood cells. Healthy people usually have 4 – 5 grams of iron stored up with about 2.5 grams of that found in the hemoglobin of red blood cells. Therefore, iron deficiency is directly caused by extensive blood loss or anemia. Most of the iron in the body is stored up until it is needed. This is because iron is a toxic mineral. Therefore, only a small amount of iron is found in the plasma either bound to transferrin or freely circulating. Iron is also found bound to proteins in the serum. In this form, it is known as ferritin. While some researchers measure ferritin levels to determine the extent of iron deficiency in ADHD subjects, other researchers have argued that serum ferritin level is not a true measure of iron deficiency and also not a good diagnostic tool for ADHD. The human body enforces a tight regulation of iron absorption and excretion. For example, as aged red blood cells break down, the body recycles their iron content. However, some iron is still lost daily in sweats, shed skin cells, and from the mucosal lining of the gastrointestinal tract. To make up for this loss, the body absorbs a little iron from diets and supplements. Dietary sources of iron include both plants and animals. Some of these sources are beans, pistachios, leafy vegetables, lentils, poultry, red meat, and fortified foods. Iron deficiency is mostly found in children and premenopausal women. For these women, the main reason is regular blood loss during menstruation. For children, iron deficiency is caused by both increased demand for the mineral and also nutritional deficiency. Because some of the symptoms of iron deficiency and ADHD overlap, scientists believe the same parts of the central nervous system are affected by both medical conditions. Some of the shared symptoms of ADHD and iron deficiency are fatigue, restlessness, and irritability. How It WorksIron acts as a co-enzyme in the anabolism of catecholamines. That implies it is necessary for the formation of certain neurotransmitters. It also helps to control the activity of the neurotransmitter dopamine, which most likely accounts for the connection of iron deficiency with neurological conditions. Thus, it makes sense that supplementing children with ADHD, having iron deficiency might alleviate their attention deficit symptoms. Another link between iron and ADHD (besides the mineral’s effect on dopamine activity in the brain) is its protective ability, especially against heavy metal poisoning. Iron reduces the absorption of such heavy metals as lead, cadmium, and mercury. Lead is of particular interest because lead poisoning is relatively common. Lead can cross into the brain and modify the activities of the dopaminergic pathway. This means that lead can reduce both the amount of dopamine released in the brain as well as inhibit the dopamine receptors. Secondly, when lead crosses into the brain, it destroys part of the blood-brain barrier and, in this way, allows substances not meant for the brain to cross over. Iron, however, is known to provide just the opposite effect on the blood-brain barrier. Iron protects the integrity of this barrier and can help reverse the damaging effects of lead. Therefore, iron has a neuroprotective effect on the central nervous system. ADHD children with iron deficiency are likelier to have their conditions worsened by lead poisoning. You may consider using ADHD supplements, such as Listol, that contain iron, to alleviate attention deficit hyperactivity disorder (ADHD) in adults and children. Case Studies of Children with ADHDA study conducted in Israel has shown promising results. It involved fourteen boys with ADHD symptoms for short-term iron administration on behavior. The boys received iron supplements daily for 30 days. After a period of 30-days, both parents and teachers of the children assessed their behavior. Parents noticed remarkable improvements in their behavior. This study suggests that hyperactive and careless behavior can be treated if the child's iron deficiency is rectified. Another study included 33 iron-deficient, but otherwise normal children. Each child was given an iron supplement and then examined by parents and teachers. The kids became less hyperactive. Thus, the study suggested that iron deficiency might cause hyperactive behavior in some children, and this behavior is reversible when the deficiency is treated. A third study involved a group of teen-aged high school girls who were found to be iron deficient. These girls were treated with iron supplementation for 8 weeks. After the 8-week study, the researchers discovered that girls who received iron supplementation performed better on memory tests and verbal learning than those who did not. As none of the studies were double-blind studies, we cannot really rely on the results. However, these studies suggest that ADHD symptoms can be alleviated with iron supplementation. Apart from behavioral problems, children with an iron deficiency are also at great risk for absorbing toxins. It has been found that children with low iron levels can easily absorb heavy metals such as lead, cadmium, and mercury. Toxicologists have also noticed an association between iron deficiency and high blood levels of lead in kids. Though the relation between iron deficiency and ADHD seems to have been determined to some extent, very few researchers have considered using it to treat the condition. If you suspect that your child might have an iron deficiency, get a blood test done to determine the mineral content and consult a doctor for the proper dosage. Iron Supplementation for ADHDIt is important to note that not everyone diagnosed with ADHD has an iron deficiency. Iron supplements should only be used in ADHD patients with measurable deficiency of the mineral. This is because too much iron is potentially toxic. Although the body has its means of regulating iron absorption, iron overload can still cause some damage. For one, too much iron can destroy the linings of the gastrointestinal tract. Too much iron circulating in the blood can also damage internal organs such as the heart and liver. Iron supplements are only advised for ADHD patients in cases where not enough can be obtained from dietary sources. When taking iron supplements, care should be taken and the iron levels in the body should be monitored. ZincZinc can contribute to behavioral changes through its regulatory effects on certain brain neurotransmitters, melatonin, and fatty acids. For ADHD therapy, it is usually given in a dose of 35 mg per day. Several studies and researches have found that children inflicted with ADHD are more likely to be zinc-deficient than other children. In this article, we will evaluate the link between zinc and ADHD. Studies and ResearchAs per a study published in Progress in Neuro-Psychopharmacology and Biological Psychiatry, taking zinc supplements can alleviate the symptoms of ADHD or attention deficit–hyperactivity disorder in children. Researchers from Iran executed a controlled clinical trial to evaluate the benefits of prescribing zinc supplements alongside the more conventional methylphenidate treatment. The study involved 44 children who were diagnosed as suffering from ADHD; none of these patients had taken any medication before the trial. For the six weeks, half the children were given zinc sulfate (55mg/day) in addition to the conventional treatment; while the other half were given a placebo. A child psychiatrist examined the children's improvements. The researchers found that children taking supplementary zinc sulfate daily showed significant improvements than those taking a placebo. Serum Zinc Levels and Hyperactivity A 2005 study published in the Journal of Child and Adolescent Psychopharmacology by 9 researchers from the Ohio State University examined the relationship between serum levels of zinc and severity of ADHD symptoms. 48 children between the ages of 5 and 10 partook in the study. The zinc serum levels for these kids were determined and then the parent and teachers' ratings of their ADHD symptoms were obtained. These parent and teacher ratings ranked the children for signs of hyperactivity and inattention. The study results showed a strong correlation between serum zinc levels and the perceived extent of ADHD symptoms. Double-blind, Placebo-controlled Study of Zinc and ADHD A 2004 study done by Turkish researchers and published in Progress in Neuro-Psychopharmacology and Biological Psychiatry examined the link between zinc deficiency and ADHD. This study involved 400 children around age 10 who were diagnosed with ADHD. Half of these children were placed on a placebo while the other half were given 150 mg of zinc sulfate daily. At the end of 12 weeks, these children were tested with the Attention Deficit Hyperactivity Disorder Scale (ADHDS), Conners Teacher Questionnaire, and DuPaul Parent Ratings of ADHD. The study’s results showed that zinc supplementation produces a more significant reduction in hyperactivity, impulsiveness, and social symptoms of ADHD than the placebo. The study did not find a marked improvement in attention span and focus after the zinc supplementation. However, better outcomes for hyperactivity symptoms were seen in older study participants who had high BMI scores and low serum levels of zinc and free fatty acids. This group of ADHD patients is believed to benefit the most from zinc supplementation. Zinc, Amphetamines, and ADHD A 1990 study published in the International Journal of Neuroscience examined how the measurement of zinc levels can help predict the effectiveness of amphetamines used in the treatment of ADHD. The study involved 18 boys between the ages of 6 and 12 who were diagnosed with ADHD. The crossover design allows the study group to switch between placebo and dextroamphetamine during the one month of the study. Response to treatment was obtained from parents’ and teachers’ hyperactivity ratings. The study measured both zinc levels in the hair and zinc levels in the urine over 24-hour periods. The results showed that the zinc measurements from hair samples provided a better indication of the efficacy of the amphetamine for treating ADHD. Also, higher zinc levels in the hair were strongly correlated with improving ADHD symptoms. These results show that ADHD children are also deficient in zinc and that zinc supplementation might help improve ADHD symptoms. Zinc and Information Processing in ADHD Children A 2008 study published in Progress in Neuro-Psychopharmacology and Biological Psychiatry examined the potential effects of zinc on information processing in 28 boys diagnosed with ADHD. The study participants were divided into two groups: those who have zinc deficiency and those who do not. 24 non-ADHD boys were used as controls. In both ADHD groups and the control group, brain activities in the regions responsible for information processing were measured using a technique called the auditory oddball paradigm. The results showed that the plasma zinc levels were lower in children in both ADHD groups than in children in the control group. Also, the control group showed better information processing than the ADHD groups. However, the group of ADHD children without zinc deficiency showed better results than the ADHD children who also had zinc deficiency. Benefits of ZincTaking zinc supplements can help combat ADHD symptoms and other disorders. Some of the benefits are as follows: It protects against the oxidative damage of omega-3 fatty acids, which can be used as potent treatment options for ADHD. Thus, taking zinc supplements alongside omega-3 treatment can help optimize the benefits and cut down the negative effects. You may consider using Listol that contains both zinc and omega-3 fatty acids. It is an effective natural supplement for alleviating ADHD symptoms in adults and children. Zinc is required to convert the inactive form of the vitamin B6 to the active pyridoxal phosphate form. Thus, a zinc supplement with vitamin B6 can help in effectively alleviating ADHD symptoms. Zinc promotes the production of melatonin, a hormone that is known to play a vital role in maintaining the important neurochemical signaling agent called dopamine. Studies have proved that zinc might be more effective in treating the hyperactive/impulsive behavior in ADHD children, than the inattentive aspect of the disorder. Zinc supplements are known to increase the effectiveness of methylphenidate (such as Ritalin), used for treating ADHD and related disorders. Natural Sources of ZincYou may also consider giving zinc-rich foods to your child to ensure that he stays healthy. Some good sources of zinc are oysters, beef, chicken, nuts, whole grains, seafood, and pork. HerbsGinsengGinseng is a slow-growing perennial herb with fleshy roots and is predominantly found in cooler climates especially in Eastern Asia and Northern America. Ginseng belongs to the plant genus, Panax. There are many Panax ginsengs including Asian ginseng, Panax ginseng itself as well as Panax quinquefolius, the American ginseng. All true ginsengs contain a group of phytochemicals called ginsenosides. Some related species such as the Siberian ginseng are not true ginsengs and do not contain ginsenosides. Ginseng is known as an adaptogenic herb. This means that it is very useful for relieving stress.
The various uses of ginseng in traditional medicine include as a stimulant, memory enhancer, and aphrodisiac. It is also used in the treatment of sexual dysfunction and type II diabetes. Ginseng also produces several positive effects on the endocrine system. For example, it stimulates the release of gonadotropins by acting on the pituitary gland. The herb also contains compounds known as phytoestrogens. However, most of the medicinal benefits of ginseng are derived from ginsenosides. Side Effects and Contraindication of GinsengGiven the fact that the phytochemicals in ginseng are active in the nervous system and cardiovascular system, the side effects of taking this herb include headache, insomnia, and changes in blood pressure. Ginseng can also cause nausea, diarrhea, nose bleeds, and breast pain.
Bleeding is the most common symptom of acute overdose of ginseng. Mild overdose will also cause dry mouth, edema, hypertension, hyperthermia, irritability, hyperactivity, insomnia, decreased appetite, itching, fatigue, and blurred vision. Gross overdose may add the following to the symptoms above: fever, decreased light sensitivity, blue/red facial discoloration, convulsion, and delirium. What are Ginsenosides?Ginsenosides are also called panaxosides. They are steroid glycosides and also saponins complexes. Ginsenosides are classified into 2 broad groups: Rb1 and Rg1. The ginsenosides in the Rb1 group are more active in the reproductive system but they are also known to increase the uptake of choline (a precursor of acetylcholine and a memory enhancer). The ginsenosides in the Rg1 group are most abundant in Panax ginseng than other ginseng species. They have been shown to improve spatial learning and increase neuronal activity in the hippocampus, one of the seats of memory in the brain. Rg1 ginsenosides are also known to prevent memory impairment by preventing the death of brain cells that could lead to dementia. Ginsenosides and Links to MemoryMost of the early studies involving ginseng and memory were done with specific ginsenosides fractions. For example, the Rb1 ginsenoside extracted from the North Africa ginseng was used to reverse the effect of scopolamine on memory. Scopolamine blocks the action of acetylcholine in the brain, and it is commonly used to induce memory deficits resembling dementia in test animals. In one study, 5 mg/kg/day of Rb1 was able to partly relieve the amnesia caused by scopolamine by stimulating the release of more acetylcholine to unblock cholinergic transmission in the brain. To increase the release of acetylcholine in the brain, Rb1 increased the uptake of choline by nerve cells especially in the hippocampus and the cortex, the two major seats of learning and memory. The secondary mechanism by which Rb1 improves memory is by preventing the neurological damage caused by reactive oxygen radicals released from lipid peroxidation in the brain. Once released these free radicals slowly destroy nerve cells and cause cognitive decline. By protecting the nerve cells, Rb1 reduces the risk of vascular accidents in the brain. GinkgoGinkgo is the name given to the herbal extract obtained from the Maidenhair Tree which is also known as Ginkgo biloba. The maidenhair tree is an ancient tree whose parts have various use in traditional medicine and as food.
Key ingredients found in ginkgo extract include terpenoids such as ginkgolides and bilobalides as well as flavonoid glycosides. These ginkgo phytochemicals are known as monoamine oxidase inhibitors. They also block the reuptake of neurotransmitters such as dopamine, serotonin, and norepinephrine. The effect of ginkgo on norepinephrine reuptake is believed to be responsible for the herb’s effects on cognition. Ginkgo is a nootropic agent. This means that it is useful for enhancing memory and concentration. However, ginkgo does not appear to improve dementia or cognitive decline in Alzheimer’s disease. The 3 proven effects that ginkgo extracts have on the body include:
Ginkgo is not recommended for people with blood circulation disorders (because of its effects on blood flow and blood clotting) and those placed on certain antidepressants (because of its effects on monoamine neurotransmitters such as serotonin). The herb should also be avoided by pregnant women. The anticoagulant properties of ginkgo also mean that it should be avoided by people placed on blood thinners such as warfarin. People who are allergic to poison ivy, cashews, and mangoes should avoid ginkgo supplements because the ginkgolic acid in the herb is related to the allergenic phytochemicals in these other plants. Common side effects of ginkgo extracts include headaches, nausea, vomiting, diarrhea, gastrointestinal discomfort, dizziness, heart palpitations, and an increased risk of bleeding. The usefulness of ginkgo extract in the restoration of cognitive function especially memory loss caused by dementia has been well studied. Over the years, the studies done on the subject have produced mixed results with some concluding there are benefits while others proving there is none. Ginkgo and Memory: The Positive ResultsIn a 2001 study published in The International Journal of Neuropsychopharmacology, the researchers administered ginkgo extract to 61 healthy study participants. The study was randomized, placebo-controlled, and double-blinded to eliminate bias.
The result of this trial showed that the ginkgo extract administered produced statistically significant improvement in working memory, information processing, and decision making. A 2005 study published in the Pharmacological Reports of the Institute of Pharmacology of the Polish Academy of Sciences investigated the benefits of ginkgo in relieving stress-induced memory loss in rats. The researchers caused post-stress memory impairment by inducing chronic stress for 2 days 21 hours or with corticosterone injections. The rats who received ginkgo extract recovered from this chronic stress and scored highest in spatial and non-spatial memory tests. Also, the administration of 100 mg/kg of ginkgo extract before stressing the rats normalized neutralized the effects of stress on memory and cognitive functions. Ginkgo and Memory: The Case against GinkgoA 2002 study published in the Journal of the American Medical Association tested the efficacy of over-the-counter ginkgo supplements for the enhancement of memory. The actual study took 6 weeks and recruited 230 healthy participants (98 men and 132 women) over the age of 60. By randomizing who gets what, each participant either got ginkgo pills or a placebo that appeared and tasted similar. The ones who got ginkgo took it according to the manufacturer’s recommendation (40 mg taken 3 times daily). At the end of the study, the participants took standardized neuropsychological tests to access improvements in verbal and non-verbal learning as well as memory, attention, and mental focus. The results showed that of the 88% of the participants who completed the study, there was no significant difference between the ginkgo group and the placebo group on any count of cognitive function including memory. Not only the standard tests but also subjective assessments by the participants’ friends and families revealed no difference between the drug group and the placebo group. In a 2004 study published in the journal, Psychopharmacology, the memory-enhancing promise of ginkgo and ginseng was accessed in a group of 126 healthy participants. This study was a subset of the larger Betula Prospective Cohort Study (3500 participants) done to understand the effects of medicinal agents on memory, health, and aging. A statistical analysis of the study showed that neither ginkgo nor ginseng improved scores in the eight memory tests done for those taking them compared to those who did not. The study concluded that there was no quantifiable benefit from a long-term supplement of ginkgo or ginseng on memory performance. A 2000 paper published in the Journal of American Geriatrics Society evaluated the possible efficacy, dose-dependence, and longevity of ginkgo extracts on dementia caused by aging. The randomized, placebo-controlled, double-blind, parallel, multicenter study recruited 214 residents of 39 old peoples’ homes. The study took 24 weeks during which each participant was given one of a placebo, the usual dose of a ginkgo extract (160 mg daily) or a higher dose (240 mg daily). 12 weeks into the trial, the participants were assessed and drug choice randomized again. The key tests in the assessment measured include verbal learning, memory span, memory status, geriatric symptoms of cognitive decline, depression, self-perception, and self-reported behavior. The results of this study showed that ginkgo supplementation did not improve the scores on any of these tests compared to placebo supplementation. Gotu KolaGotu kola is an adaptogen. This means that it can help the body cope with stress by reducing the levels of stress hormone and calming down the rapidly firing neurons in the brain. However, it has other medicinal benefits. Gotu kola is also traditionally prescribed as a brain tonic. This is because of its potent nootropic effects. This herb increases blood circulation in the brain and has been shown, in multiple clinical trials, to be useful for improving memory and cognition especially in the elderly. Green TeaGreen tea is native to China and a staple drink in most of Asia. It is made solely from the leaves of Camellia sinensis which have undergone only a little oxidation during processing. A lot of factors can affect the relative composition of the phytochemicals of green tea leaves. For example, the quality of green tea depends on the soil on which it is grown, the climate of the area, when it is harvested, and how it is processed. In recent years, green tea is also becoming popular in the West where black tea has been the traditional tea of choice. This shift is due to the increasing number of studies that are showing the health benefits (and oftentimes, the superiority) of green tea. The flavonoid content of tea is one example of the phytochemicals that make it a healthful drink. It has been calculated that the flavonoid content of green tea surpasses those of fruits, vegetable juices, and wine. Flavonoids are prized phytochemicals because of their anticarcinogenic and antioxidant properties. These and other beneficial phytochemicals in green tea have been demonstrated to help reduce the risks of certain cancers and heart disease. Some of the other healthful phytochemicals in green tea are vitamin C, carotenoids, and tocopherols as well as zinc, selenium, chromium, and manganese. Another important group of phytochemicals found in green tea is polyphenols. Of polyphenols, catechins are the most important and of catechins, epigallocatechin gallate is the most abundant. Besides its ability to reduce the risks of some cancers and heart disease, both animal and human studies have also demonstrated that green tea is useful in the treatment of rheumatoid arthritis, dental cavities, bone loss, and kidney stones. Other benefits of green tea include improving immune function and reducing blood pressure, LDL (“bad” cholesterol), and total cholesterol levels. Green tea (especially if it has high polyphenol content) also increasing thermogenesis and can, therefore, help reduce fat storage and weight gain. Green tea is also shown to help learning and memory as well as other aspects of cognitive functioning. Different studies have identified that the active compound in green tea responsible for its neuroprotective properties is epigallocatechin gallate or EGCG. It is known to protect brain cells from dying and restoring damaged neurons. What is Epigallocatechin Gallate?Epigallocatechin gallate is the most abundant catechins in green tea. Black tea does not contain epigallocatechin gallate because the phytochemical is converted to other compounds during processing. EGCG is a powerful antioxidant. It is available as an ingredient in many supplements. The therapeutic uses of EGCG are mainly due to this antioxidant property. It is used to reverse dementia either caused by AIDS or neurodegenerative diseases such as Alzheimer’s. EGCG is also used in cancer treatment, to treat chronic fatigue and muscular atrophy. How Green Tea Improves MemoryWhile it has been long known that the antioxidant property of some of the phytochemicals in green especially EGCG is beneficial for memory, some new studies are showing other benefits for EGCG in the brain. Antioxidant Effect EGCG as an antioxidant protects the neurons from damage caused by reactive oxygen species and other harmful free radicals. This protection allows nerve cells to continue working and for neuronal transmission to proceed normally. This effect prevents cognitive decline and is especially beneficial if the damage to brain cells is not permanent or extensive. However, the secondary mechanism by which the EGCG in green improves memory and learning may help explain why green tea can reverse cognitive decline and improve memory even in healthy people. Neurogenesis In a study published in the journal, Molecular Nutrition and Food Research in 2012, Chinese scientists were able to demonstrate that EGCG can stimulate neurogenesis in the brain. Unlike the antioxidant protection provided by EGCG, neurogenesis is a proactive mechanism of action of this green tea phytochemical. Neurogenesis refers to the generation of new brain cells. It is important because it can help improve brain function. While free radicals kill off brain cells, neurogenesis turns up a new generation of these cells. When the rate of neurogenesis exceeds the rate at which free radicals damage brain cells, the net result is maintenance or improvement in cognition. In this study, the researchers were able to demonstrate that EGCG stimulated neurogenesis in the hippocampus, a prime area of the brain involved in learning and memory. EGCG increased the production of neural progenitor cells which behave like stem cells because they can be turned into any kind of brain cells. Even though this study involved mice, the same effect likely applies to humans. This study demonstrates that ECGC (and by extension, green tea) improves memory and other aspects of cognition by promoting neurogenesis and by protecting nerve cells by their antioxidant properties. Acetylcholinesterase Inhibitor In an earlier study published in the journal, Bioscience, Biotechnology, and Biochemistry in 2004, researchers demonstrated that the polyphenol extract of green tea improved memory and cognition by inhibiting the enzyme known as acetylcholinesterase. Acetylcholinesterase is the enzyme that breaks down the neurotransmitter, acetylcholine in the brain. Given the importance of acetylcholine and the cholinergic pathway to learning and memory, increased acetylcholinesterase activity can reduce the quality and span of memory. As we age, this effect becomes even more important because acetylcholine production declines with age. To improve cholinergic activity in old age, drugs that inhibit acetylcholinesterase can have profound effects on learning and memory by preventing cognitive decline. The polyphenols in green tea do inhibit acetylcholinesterase, and therefore, they can prevent short-term memory loss especially in the elderly and those suffering from neurodegenerative diseases such as Alzheimer’s. MRI EvidenceIf green tea can indeed improve memory it must cause discernible changes in the areas of the brain responsible for cognition. This hypothesis was tested by some researchers who published their findings in the European Journal of Clinical Nutrition. The neuroimaging method used was MRI (magnetic resonance imaging). This imaging technique was used on human subjects who took a whey-based beverage containing green tea. The brain imaging result showed that green tea lit up an important area of the cortex. More specifically, the polyphenol content of green tea was linked with increased activation of the dorsolateral prefrontal cortex which is the part of the brain responsible for working memory. Bacopa
Although it is native to the marshy areas of India, Sri Lanka, Nepal, China, and Vietnam, bacopa is also grown in the wetlands of the Southern US as well as Hawaii and Florida. Bacopa is an important remedy in Ayurveda medicine. In that practice of traditional medicine, the herb is used to treat several diseases including ulcers, epilepsy, asthma, inflammations, tumors, anemia, leprosy, and an enlarged spleen. It is also used as a memory enhancer. The phytochemicals present in bacopa include alkaloids, saponins, flavonoids, stigmasterol, beta-sitosterol, and bacopa saponins. These compounds give bacopa its medicinal properties. For example, bacoside A, a bacosaponin, is responsible for most of the antioxidant effects of bacopa. This compound improves the activities of some antioxidant enzymes (superoxide dismutase, catalase, and glutathione peroxidase) naturally produced in the body. Other active ingredients of the herbs such as the polyphenol compounds are also known to confer antioxidant properties. The polyphenols, for example, cut off the chain reaction of oxidative stress in the body by mopping up reactive oxygen species, neutralizing toxic metallic ions, and inhibiting the enzyme that produces harmful free radicals from lipid metabolism. The combination of these antioxidant properties is believed to be responsible for the ability of bacopa extract to improve the symptoms of Alzheimer’s disease by removing the beta-amyloid proteins deposited on neurons in the brain. Various studies done with animal models indicate the bacopa extracts are effective for increasing memory capacity and for reversing cognitive decline in the elderly. Besides its effect on cognition, bacopa can also increase the production of immunoglobulins and regulate the production of antibodies. Therefore, this herb can improve the functioning of the immune system. However, bacopa is not without its side effects. It is known to reduce heart rate and increase secretions in the stomach, intestines, and urinary tract. These side effects are usually mild and should only cause mild gastrointestinal discomfort. Bacopa can also cause dry mouth and muscle fatigue. Still, bacopa should be used with caution by those who have ulcers and urinary tract problems. Also, bacopa enhances the effect of a group of antihypertensive drugs known as calcium-channel blockers. Therefore, where both drugs are to be used, the dose of the antihypertensive drug should be reduced. How Bacopa Improves Memory and Cognitive FunctioningStill, the most in-depth work on bacopa and its effects on the brain is done by Indian scientists who are driven by the legacy of this Ayurvedic remedy. In a study published in the journal, Phytotherapy Research, Indian researchers were able to provide evidence for the antioxidant effect of bacopa on the hippocampus in rats. Given that the hippocampus is one of the parts of the brain dedicated to memory and learning, it is clear to see how bacopa may improve memory and cognition. By protecting the neurons and neurotransmitter pathways passing through the hippocampus, bacopa can help preserve their integrity and even reverse cognitive decline. Reactive oxygen species, free radicals, and harmful proteins such as beta amyloids can destroy nerve cells and interfere with the signal transmission in the brain. When these destructive toxins affect the hippocampus and other memory seats of the brain, they can start the neurological degeneration that later presents as memory loss and cognitive decline. To prevent this destruction, the body needs antioxidants to neutralize and remove these harmful compounds. Bacopa easily supplies such antioxidants. In fact, given the number of potent antioxidants present in bacopa, it is no wonder that it has such dramatic results in every one of the studies investigating its efficacy in preventing and reversing cognitive decline. Furthermore, this antioxidant effect explains why bacopa does not affect memory and cognitive performance in healthy subjects. Where there is no sign of cognitive decline caused by damage to the hippocampus, bacopa cannot improve in a normal situation. A 1996 paper published in the Indian Journal of Experimental Biology tries to explain the mechanism behind the antioxidant properties of bacopa. Among other things, the authors of this paper believed that the antioxidant compounds in bacopa work in multiple pathways. When compared to known antioxidants such as vitamin E (natural) and EDTA (synthetic), bacopa extract performed similarly to them. It was able to chelate reactive metal ions (like EDTA) and break the chain reaction that produces free radicals during lipid peroxidation (like vitamin E). The paper concluded that under experimental conditions, the results showed that 100 micrograms of bacopa extract were equivalent to 247 micrograms of EDTA and 58 micrograms of vitamin E. Just as importantly, the researchers discovered that the antioxidant benefits of bacopa increased as the dose of the extract is increased. Huperzia
Huperzine A protects the brain from damage caused by both beta-amyloid proteins and glutamate. It increases the production of nerve growth factors to speed up neurogenesis and also blocks acetylcholinesterase. With such multiple mechanisms of action, huperzine A is one of the well-received phytochemicals for treating memory loss and cognitive decline. AshwagandhaAshwagandha is also known as Indian ginseng and it is traditionally used in Ayurveda medicine to treat cognitive disorders. Its effects mirror those of huperzia because it also protects against beta-amyloid proteins while promoting neurogenesis. Other Natural SupplementsL-Carnitine and ALCARL-carnitine is another commonly used supplement for enhancing memory. It is synthesized from the two amino acids, methionine, and lysine. Carnitine is an antioxidant compound that has also been proven to improve mental focus and memory. ALCAR or acetylcarnitine is a derivative of this molecule. ALCAR has a better absorption profile than carnitine and it crosses the blood-brain barrier more easily. It shares the same medicinal properties as carnitine and is also used to improve memory and cognitive function in patients with neurodegenerative disorders. CholineCholine refers to a group of water-soluble, quaternary ammonium salts. It is an essential nutrient and is also sometimes classified as part of the B vitamins. Choline is especially renowned as a precursor of acetylcholine, an important neurotransmitter in the brain involved in memory, muscle activities, and other functions. Choline is also essential in the body because it is used to make structural components (phospholipids) of cell membranes. Since the human body only makes a small amount of choline, dietary sources of the nutrient are very important. The recommended adequate intake value for choline varies by age and sex. Children normally require 125 – 250 mg/day. Adult males need 550 mg/day of choline while adult females need 425 mg/day. The upper limit for choline is 3500 mg/day for adults, 3000 mg/day for teenagers, and 1000 mg/day for children. The choline demand by the body increasing during pregnancy and lactation. This is because choline is essential to support the development of the nervous systems of fetuses and infants. Therefore, the recommended daily intake of choline for pregnant women is 450 mg/day and for lactating women, the value is 550 mg/day. Excellent dietary sources of choline include raw beef liver, hardboiled egg, chicken, codfish, cauliflower, wheat germ, low-fat milk, soy lecithin, tofu, spinach, almonds, peanuts, and cooked brown rice. Given that choline is required for the structural integrity of cell membranes, for cellular communication, and for synthesizing acetylcholine, its deficiency can have some serious effects. Signs of choline deficiency include growth impairment, hypertension, and infertility. This deficiency will also cause bone abnormalities, fatty liver, and liver necrosis. Choline deficiency has also been shown to cause and increase carcinogenic activities in the body. Although it is estimated that most of the population consumes less than the recommended daily intake of choline, those at the greatest risk of choline deficiency include vegans, vegetarians, and endurance athletes. Drinking a lot of alcohol can also cause choline deficiency. Choline Dietary SupplementsThere are different forms of choline supplements. The most popular source of choline supplementation is the food additive, lecithin, derived from either soy or egg yolks. Phosphatidylcholine is another supplementary source of choline. It is sold as a pill and powder. However, it is choline chloride and choline bitartrate that is usually referred to as choline supplements. The chloride salt is usually preferred because it does not have the gastrointestinal side effects of phosphatidylcholine. Also, an infant formula that is not prepared from cow’s milk is required to add choline. Several studies in different animal models have proven that choline supplementation during pregnancy can improve cognition in offspring. However, care should be taken with choline supplementation in pregnant women who smoke because while choline supports and protects certain parts of the brain, it actually causes brain damage in some other parts when combined with nicotine. The choline supplied to the body in supplements can easily cross the blood-brain barrier. Choline may be insoluble in lipids but a special transporter ferries it across and into the brain where it can enhance memory and other aspects of cognition. Choline supplements are also sometimes used as drugs in the treatment of glaucoma, atherosclerosis, hepatitis, Alzheimer’s disease, bipolar disorders, and other neurological disorders. Choline is also a common supplement to help those suffering from alcoholism. Choline Consumption and Memory Scores in AdultsThe benefits of choline on cognitive development are not restricted to infants and children. Several studies have also established that choline consumption in adults can have a marked difference in memory and other aspects of cognition. In one study done by researchers from the Boston University School of Medicine, the dietary data of a group of 1400 adults between the ages of 36 and 83 were examined. The data was gathered between 1991 and 1995, and then the group was given memory tests and MRI brain scans between 1998 and 2001. The researchers discovered that adults who ate choline-rich foods scored highest in the memory tests. To remove any other contributing factors, the researchers corrected for the consumption of fats, neuroprotective vitamins such as vitamins B6 and B12 as well as caloric intake and even the subjects’ education. Even after then the results still showed that the subjects who ate choline-rich diets performed significantly better than those who did not. Furthermore, the choline-eating subjects had a lesser chance of developing white matter hyperintensity (seen from the MRI scans). This is a form of brain damage caused by weakened vessels and known to cause dementia and increase the risk of stroke. In a smaller but more direct study done by researchers at Florida International University, 41 subjects between the ages of 50 and 81 were given 500 mg of choline (in the form of lecithin granules) daily for 5 weeks. After the supplementation, the group improved in memory tests (everyday memory tasks such as name recollection, etc.) more than those who did not receive choline supplements. The results revealed that choline supplementation was able to reduce memory lapses from an average of 35 per week to 19. Even though choline can help improve memory in adults, experts are quick to warn that the best benefits of choline are obtained when given early in life while brain development is still rapid and before some aspects of brain functioning are set in place. The major challenge of choline supplementation in adults is getting choline into the brain. The transporter responder for ferrying choline across the blood-brain barrier has a low affinity and is, therefore inefficient. Therefore, it is possible to increase blood levels of choline in adults without seeing an attendant improvement in cognitive function especially where neurodegenerative disorders, such as Alzheimer’s disease, are already in progress. Omega-3 Fatty AcidsOmega 3 fatty acids are polyunsaturated acids that have surprisingly large health benefits. Omega 3 fats can reduce inflammation, lower blood pressure, improve the immune system, reduce blood clotting, and even improve arthritis symptoms. Research also suggests that these necessary fats are also beneficial in reducing symptoms of ADHD. Broken down, omega 3 fats have three types: ALA, DHA, and EPA. The body cannot make these fats on its own but uses them for many of the body's processes, which is why they are so essential. The U.S. National Academy of Sciences recommends that adults and children consume about one or two grams of omega 3 fats per day. One serving of fish only has 0.2 grams, which means you'll need a lot of fish every day to get to optimal levels. Most Americans find it much easier to supplement with fish oil capsules to ensure they receive enough omega 3 fats daily. The Study FindingsIn The Netherlands study from 2015, researchers examined the effects of omega 3 supplementations on boys with and without ADHD. Most of the boys with ADHD were also taking stimulant medication. For 16 weeks, all children took omega 3 supplements. The children took an attention test before and after the trial period. Both groups of boys had improved attention scores after supplementing with omega 3s. However, the boys with ADHD improved the most with their scores increased by nearly two points. Boys without ADHD only improved by 0.1 points. How can Omega 3s Benefit ADHD? Studies show that omega 3 fats can have a positive effect on ADHD symptoms. According to a child and adolescent psychiatrist at The Children's Hospital of Philadelphia, Dr. Anthony Rostain, the findings in recent studies "helps to confirm what we already know." Research has indicated for quite a while that omega 3 can influence ADHD symptoms. Researchers are not sure how omega 3s benefit ADHD symptoms, except that they promote brain health and functioning. ADHD is a neurological disorder in the brain that is usually treated with stimulant medication that helps the brain function properly. If omega 3 fats have a similar effect on boosting brainpower, it makes sense that they could reduce ADHD symptoms. Previous research has also found that children with ADHD tend to be lower in omega 3 regardless of how much they consume. This also suggests that children with ADHD have trouble processing nutrients of any kind. However, omega 3 supplements only usually show moderate improvement in ADHD symptoms rather than a dramatic improvement. Symptoms are controlled best when a multi-faceted approach is implemented, which can include other supplements, diet changes, and behavior therapy. How to Add Omega 3 to Your DietThere are two ways to add omega 3 to your diet: food or supplements.
Supplements come in a variety of forms, but most researchers suggest looking for supplements that are high in DHA and EPA rather than ALA, which must be converted to the other two forms of omega 3 before it can be used. Children can start taking one capsule per day and gradually increasing to an adult dose twice a day, watching for any signs of reactions. For best results, combine omega 3 supplements with other natural treatments for ADHD. Omega 3 Can Help ADHDNumerous studies indicate that omega 3 supplementations can be highly effective in reducing ADHD symptoms. Parents who are not ready to turn to medication for their children, or who want to avoid it altogether, can use omega 3 supplements combined with other vitamin and mineral supplements to regulate ADHD naturally and prevent attention problems and emotional outbursts. In many cases, it may not be necessary to turn to addictive ADHD medication at all. Sourceshttp://www.webmd.com/vitamins-and-supplements/lifestyle-guide-11/fortifying-your-memory-with-supplements http://www.memory-improvement-tips.com/vitamins-for-memory.html#supplements http://www.pnas.org/content/108/8/3103
[+] Show All
|
||
| Next Article: ADHD & GABA - Will it Help? |





 The more specific benefits of B
The more specific benefits of B  Like the B vitamins, they protect the neurons in the brain from structural damage. However, they work by a different mechanism.
Like the B vitamins, they protect the neurons in the brain from structural damage. However, they work by a different mechanism. To avoid the depletion of the calcium store of bones, the parathyroid hormone regulates the rate at which it is released from bones, prevents its loss in the kidneys by promoting its reabsorption back into blood circulation, and increases the absorption of more calcium from the gut by activating vitamin D3.
To avoid the depletion of the calcium store of bones, the parathyroid hormone regulates the rate at which it is released from bones, prevents its loss in the kidneys by promoting its reabsorption back into blood circulation, and increases the absorption of more calcium from the gut by activating vitamin D3. Stomach bleeding and increased risk of cardiovascular diseases and some cancers are some of the serious side effects of long-term use of calcium channel blockers. However, brain damage and memory loss are now added to that list.
Stomach bleeding and increased risk of cardiovascular diseases and some cancers are some of the serious side effects of long-term use of calcium channel blockers. However, brain damage and memory loss are now added to that list. For those who eat calcium-poor diets, over-the-counter calcium supplements may be of help at least to reverse hypocalcemia and improve memory. However, since calcium affects memory in ways beyond just increasing calcium levels in the brain, the gains of calcium supplementation may be moderate in reversing calcium loss.
For those who eat calcium-poor diets, over-the-counter calcium supplements may be of help at least to reverse hypocalcemia and improve memory. However, since calcium affects memory in ways beyond just increasing calcium levels in the brain, the gains of calcium supplementation may be moderate in reversing calcium loss. Both the leaves and roots of ginseng contain medicinal compounds. However, the root is the most commonly used plant part in traditional medicine. Therefore, ginseng is usually sold as a dried root herb that can be added to tea and beverages. It is an ancient traditional remedy that is still used for the same purposes today.
Both the leaves and roots of ginseng contain medicinal compounds. However, the root is the most commonly used plant part in traditional medicine. Therefore, ginseng is usually sold as a dried root herb that can be added to tea and beverages. It is an ancient traditional remedy that is still used for the same purposes today. Ginseng should not be taken along with antidepressants such as phenelzine (the combination is known to cause mania). It should not also be taken with anticoagulants such as warfarin (the combination will cause excessive bleeding).
Ginseng should not be taken along with antidepressants such as phenelzine (the combination is known to cause mania). It should not also be taken with anticoagulants such as warfarin (the combination will cause excessive bleeding). The leaves of ginkgo provide the most medicinal benefits of the various parts of the tree.
The leaves of ginkgo provide the most medicinal benefits of the various parts of the tree. After 30 days of supplementation with ginkgo, the study subjects were given the same set of standard neuropsychological tests that they took at the beginning of the trial.
After 30 days of supplementation with ginkgo, the study subjects were given the same set of standard neuropsychological tests that they took at the beginning of the trial.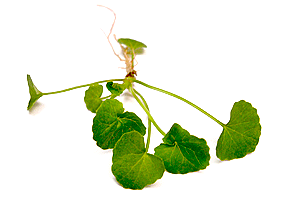 Bacopa is a perennial, creeping herb also known as Brahmi and Water hyssop. Its scientific name is Bacopa monnieri.
Bacopa is a perennial, creeping herb also known as Brahmi and Water hyssop. Its scientific name is Bacopa monnieri. Huperzia contains the increasingly popular active ingredient known as huperzine A. This phytochemical is currently in clinical trials as a drug candidate for treating Alzheimer’s disease.
Huperzia contains the increasingly popular active ingredient known as huperzine A. This phytochemical is currently in clinical trials as a drug candidate for treating Alzheimer’s disease.